Abstract
Background: Haplo-identical stem cell transplantation is increasingly been used in recent years in the treatment of acute leukemia. In particular, the use of T-cell replete grafts with post-transplant cyclophosphamide (PTCy) for prevention of graft-vs-host disease (GVHD) is becoming a valid treatment option with encouraging outcome. The initial studies used bone-marrow as the stem-cell source, but more recently, peripheral blood stem cells (PBSC) are also used. There is more limited data on the prognostic factors following haplo-identical transplantation with PBSC. Natural killer (NK) allo-reactivity as predicted by missing killer-cell immunoglobulin-like receptor (KIR) ligands in the recipients that are present in the donors has been shown to be an important factor in the outcome of T-cell depleted haplo-identical transplants. NK alloreactivity is associated with reduced relapse risk and improved survival in patients with AML, but not in patients with adult ALL. In addition, patients with donor NK alloreactivity had better engraftment and lower risk of GVHD. The role of NK cell allo-reactivity in the setting of T-cell replete haplo-identical transplant with PBSC and PTCy is unknown.
Patients and Methods: The study included 238 patients, 139 male, 99 female, median age 45 years (range, 18-78) with AML (n=176) or ALL (n=62) who had T-replete haplo-identical transplant with PTCy between the years 2010-2015. All patients were given PBSC as their stem cell source. Patients were in CR1 (38%), CR2 (24%) or active disease (38%). Conditioning was myeloablative (47%) or reduced-intensity (53%). GVHD prevention included cyclosporine or tacrolimus with mycophenolate, in addition to PTCy, in 82%. KIR-ligand mismatching was predicted according to patient and donor HLA typing and correlated with transplantation outcomes. In all, 89 patients (37%) had a KIR mismatch in the GVHD direction, based on missing expression of C1, C2 or Bw4 ligands in the recipients that were expressed in their donors. There was no significant difference in patient characteristics between the group with and without KIR mismatch.
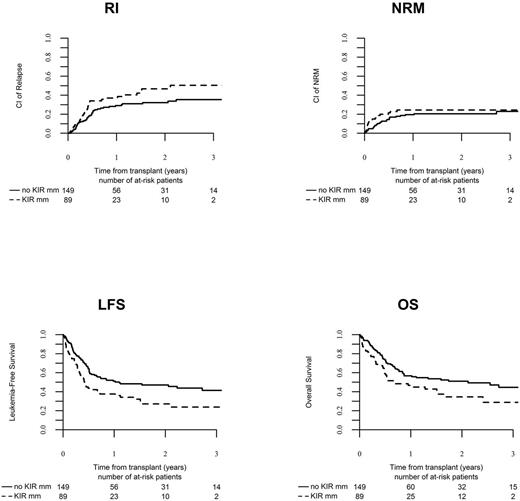
Results: The median follow-up was 14 months (range, 1-50). Ninety-four percent of patients engrafted. The 2-year relapse and non-relapse mortality (NRM) rates in the entire group were 36% (95%CI, 29-42) and 22% (17-27), respectively. The leukemia-free (LFS) and overall survival (OS) rates were 43% (36-50) and 49% (42-56), respectively. Acute GVHD grade II-IV and chronic GVHD occurred in 34% (29-40) and 32% (26-39), respectively. The 2-year OS was 35% (22-47) in patients with KIR mismatch and 51% (42-60) in patients with no KIR-ligand mismatching (P=0.02). 2-year LFS rates were 27% (16-38) and 47% (38-56), respectively (P=0.003). Multivariate analysis identified AML (compared to ALL) (HR 0.51, P=0.008), active disease at transplantation (HR 5.03, P<0.001) and KIR mismatching (HR 1.60, P=0.03) as factors associated with 2-year OS. A center effect was also identified (P=0.05). The same factors predicted for LFS. KIR mismatching was associated with a higher incidence of relapse, 47% (34-58) and 32% (24-41), respectively (P=0.05). Multivariate analysis identified active disease at transplantation (HR 6.38, P<0.001), KIR mismatching (HR 1.97, P=0.03), female donors (HR 0.58, P=0.03) and reduced-intensity conditioning (HR 1.71, P=0.05) as factors associated with 2-year relapse. KIR mismatching was not associated with NRM, acute or chronic GVHD.
Conclusions: Haplo-identical transplant with PTCy and PBSC graft is associated with favorable outcome in patients with acute leukemia. KIR ligand mismatching may be associated with increased relapse rate and worse survival in these patients. Donors with KIR mismatching should be avoided when possible in the PBSC haplo-identical setting.
Ciceri: GSK: Other: B-thalassemia gene therapy was developed by Fondazione Telethon and Ospedale San Raffaele and has been inlicenced by GSK that provides funding for the clinical trial, Research Funding. Mohty: Sanofi: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal